Abstract
Introduction:
Allogeneic hematopoietic stem cell transplantation (HSCT), can be curative for many hematologic disorders. However, HSCT is still associated with significant risks. HSCT outcomes are dependent on patient, disease and transplant related factors. There are a number of assessment tools being used to predict outcomes. Some use patient related variables such as the hematopoietic cell transplantation specific comorbidity index (HCT-CI), some use disease-related variables such as the disease-risk index (DRI) and some others incorporate combined variables. We aimed to incorporate disease, patient comorbidities, donor, and transplant characteristics into one comprehensive prognostic model to predict 2 year disease-free survival (DFS).
Methods:
273 consecutive patients (162 males, 111 females) receiving an initial HSCT from 2010 and 2016 were identified and retrospectively analyzed. Median age was 56 years (range 18-76 years) and a broad representation of hematologic disorders (119 AML, 46 ALL, 60 MDS, 18 NHL, 30 other) were included. All pts received peripheral blood as graft source. The majority received an unrelated donor transplant (166) and were conditioned with a myeloablative regimen (199).
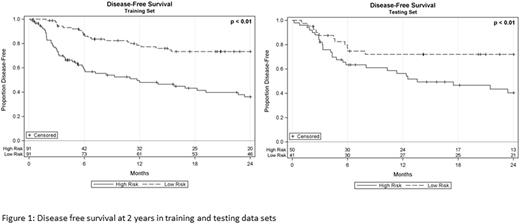
The dataset was randomly split in a 2:1 ratio to create training and testing dataset prior to data analysis. Variables under consideration as predictors of 2 year disease-free survival included: patient (age, sex, blood type, CMV status, Karnofsky Performance Status, HCT-CI), donor (age, sex, blood type, CMV status), disease (type, time since diagnosis, Disease Risk Index), and transplant (prep regimen, year of transplant, related/unrelated, match/mismatch) characteristics. Using the training dataset, a lasso penalized Cox regression was applied with the penalty parameter being derived as the mean of 1,000 iterations of 10-fold cross-validation. Patient risk scores was computed from the model and used to stratify patients based on a median split of risk scores; survival differences were evaluated using the log-rank test. Model performance was evaluated in the training and testing datasets by deriving time-dependent AUC curves, evaluating survival differences by risk strata, and comparing predicted to observed survival probabilities at 2 years.
Results:
Karnofsky Performance Status (<90, 90+), Disease Risk Index (Low, Intermediate/High), HCT-CI (Low, Intermediate/High), prep regimen (RIC/Non-myeloablative, myeloablative), and donor age (<30, 30+) were selected by the model. More specifically, lower performance status (HR 1.3), higher Disease Risk Index (HR 1.4), higher HCT-CI (HR 1.3), RIC/non-myeloablative prep regimen (HR 1.1), older donor age (HR 1.1) were associated with poorer disease-free survival. The prognostic model derived from the training dataset demonstrated good discrimination for the prediction of 2 year DFS with a median AUC value of 0.72 (IQR 0.69-0.73). When applied to the testing dataset, an AUC value of 0.73 was obtained. Across time, results were relatively consistent between 1 and 2 years post-transplant. A significant difference between the two risk strata was evidenced in the training and testing dataset (Figure 1, p<0.01). Comparison of predicted and observed survival probabilities at 2 years demonstrated agreement in both datasets.
Conclusion:
This comprehensive prognostic model is able to stratify patients into high risk and low risk groups with significantly different outcome. The inclusion of additional variables in the model increased accuracy (higher AUC) relative to existing models, which highlights the importance of taking into consideration additional constructs when trying to predict DFS. Further independent validation of our findings is necessary.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.